Anju Goel, MD, MPH, is a board-certified physician specializing in public health, infectious diseases, diabetes, and health policy.
Penicillin is an antibiotic used to treat certain types of bacterial infections.Common side effects include diarrhea and upset stomach, and some people may have an allergic reaction to penicillin — effects range from mild to severe.
Penicillin can be given by mouth, or injected intravenously (IV, into a vein), or intramuscularly (IM, in a large muscle).And there are different types of penicillins with different mechanisms of action.
All forms of penicillin are derived, at least in part, from a fungus called Penicillium chrysogenum.
Scottish scientist Alexander Fleming discovered penicillin in 1929 when he realized that bacterial cultures accidentally contaminated with “mold juice” were being killed by the fungus.It wasn’t until 1941 that scientists were able to successfully isolate, purify and test the drug on their first patient, ushering in the era of antibiotics.
By the 1960s, scientists were able to develop the first semisynthetic penicillin drug capable of treating a wider range of bacterial infections.Around the same time, they began to recognize the threat of penicillin resistance, in which mutant strains resistant to the antibiotic began to emerge and spread throughout the population.
Today, an increasing number of bacterial infections are fully or partially resistant to the original penicillin drugs, including Neisseria gonorrhoeae (gonorrhea) and methicillin-resistant Staphylococcus aureus (MRSA).
Streptococcus pneumoniae, a type of bacterial pneumonia, as well as some types of Clostridium and Listeria are also becoming less responsive to these antibiotics.
Overuse of antibiotics to promote growth in livestock is known to increase the risk of drug-resistant bacteria, including superbugs, throughout the food chain.Due to this growing global concern, the United States banned the use of antibiotics to promote animal growth in 2017.
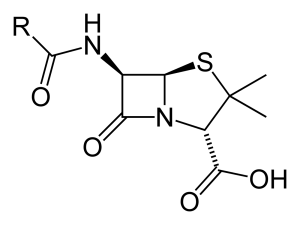
Penicillins belong to a larger family of drugs called beta-lactam antibiotics.These drugs have a similar molecular structure, consisting of a ring of four atoms called beta-lactams.Each type of penicillin has additional side chains that determine its activity.
Penicillin works by binding to molecules on the bacterial wall called peptidoglycan.When bacteria divide, penicillin prevents the normal reorganization of proteins in the cell wall, causing the bacterial cells to rupture and die rapidly.
Natural penicillins are those extracted directly from the P. chrysogenum fungus.There are two natural penicillins.
Semi-synthetic penicillin is produced in the laboratory and is similar to the chemical found in P. chrysogenum.There are four classes of semisynthetic penicillins, including commonly used antibiotics such as amoxicillin and ampicillin.
Each of these types has a slightly different molecular structure and may be administered differently than the other types.
Some penicillins have no direct antibacterial activity.They are used in combination therapy to help overcome penicillin resistance.For example, clavulanic acid blocks an enzyme secreted by antibiotic-resistant bacteria (beta-lactamase) that inhibits the activity of beta-lactam antibiotics.
Penicillins are used to treat bacterial infections – they do not treat viral, fungal or parasitic infections.These drugs are usually effective against Gram-positive bacteria, a class of bacteria that have peptidoglycan on the outside of their cell walls.For Gram-negative bacteria, the peptidoglycan layer is buried under a layer of lipid cells, making it harder for drugs to access the molecule.
Gram-positive bacteria that can be treated with penicillin include Clostridium, Listeria, Neisseria, Staphylococcus, and Streptococcus.
Natural penicillins – penicillin G and penicillin V – are still used today for the treatment of some common and uncommon bacterial infections.
In contrast, semisynthetic antibiotics like amoxicillin—one of the most commonly used antibiotics today—are used to treat a wide range of respiratory, skin and bacterial infections such as H. pylori, Lyme disease and acute otitis media.
Off-label use of penicillin is common, although drugs such as amoxicillin and ampicillin are more common than natural penicillin.Off-label use includes treatment of intensive care patients with sepsis or neonates with acute respiratory distress.In neither case, these drugs are used for such purposes, but they are generally considered necessary when no other treatment options are available.
Penicillin G is sometimes used off-label to treat prosthetic joint infections, Lyme disease, and leptospirosis.Penicillin V is occasionally used off-label to treat Lyme disease and otitis media, or to prevent infections in people receiving stem cell transplants.
Penicillin can be very effective when used properly.Even so, in some cases, the drug is not effective at clearing the infection.In this case, antibiotic susceptibility testing (also called antibiotic susceptibility testing) can be used to determine whether a person’s infection is responsive to penicillin.
The test begins by culturing bacteria taken from swabs of bodily fluids and then exposing the bacteria directly to various types of penicillin in the laboratory.Antibiotic susceptibility testing is commonly used in patients with community-acquired pneumonia who have severe illness or are at high risk of death.
Penicillin is contraindicated if you have previously been allergic to any drug in the penicillin family.You should also be cautious if you have had a severe drug hypersensitivity reaction in the past, including anaphylaxis, Stevens-Johnson syndrome (SJS), or toxic epidermal necrosis (TEN).
If you have had an allergic reaction to penicillin G or penicillin V in the past, you may (but not necessarily) be allergic to semi-synthetic penicillins such as amoxicillin or ampicillin.
People allergic to penicillin should use other beta-lactam antibiotics with caution because of the risk of cross-reactive allergy, although the risk is small.This includes cephalosporin antibiotics such as Keflex (cephalexin), Maxipime (cefepime), Rocephin (ceftriaxone), and Suprax (cefixime).
If you are concerned that you may be allergic to penicillin, you can have a skin allergy test to see if you have a reaction to the tiny amount of the drug placed under your skin.
Penicillin should also be used with extreme caution if you have acute renal (kidney) failure.Penicillin is primarily excreted by the kidneys, and decreased renal function can lead to accumulation of the drug to toxic levels.The consequent overdose of penicillin can lead to symptoms of agitation, confusion, coma, abnormal convulsions, and, in rare cases, coma.
The recommended doses of penicillin G and penicillin V may vary depending on the disease and the age of the person being treated.
Depending on the recipe, the dose is measured in several different ways.In adults, drugs are usually measured in units or milligrams (mg).In children, doses can be calculated in milligrams per kilogram of body weight per day (mg/kg/day) or in units per kilogram of body weight per day (units/kg/day).
If you have kidney disease, you may need to lower your penicillin dose to prevent drug toxicity.When creatinine clearance (a measure of kidney function) falls below 10 milliliters per minute (mL/min), dose reduction is usually recommended.
On the other hand, if you are on hemodialysis, you may need a higher dose because hemodialysis can speed up the removal of penicillin from your blood.
Penicillin G is available as a premixed solution or as a powder for reconstitution with Sterile Water for Injection.Premixed solutions can be stored in the refrigerator or freezer, while powder formulations can be stored safely at room temperature.
Penicillin V is available as an oral tablet or as a cherry-flavored powder mixed with water.Both are safe to store at room temperature.Once the powder has reconstituted, it should be stored in the refrigerator and discarded after 14 days.
Penicillin V should be taken on an empty stomach to ensure maximum absorption.It should be taken at least one hour before or two hours after a meal.
If you miss a dose of penicillin V, take it as soon as you remember.If it’s nearing time for your next dose, skip the dose and continue taking it as usual.Never double the dose.
Always take penicillin as directed and done.Don’t stop just because it feels good.You need to complete the entire course in order to eradicate all germs.Once treatment is stopped, a small amount of remaining bacteria can multiply.
Most penicillin side effects are mild and transient and resolve on their own without treatment.But sometimes the side effects can be severe, even life-threatening, and require urgent care.
One of the most serious problems associated with penicillin use is the risk of a potentially life-threatening systemic allergic reaction called anaphylaxis.Allergic reactions to true penicillin affect about 1 to 5 people in 100,000.
An allergic reaction can cause serious harm if left untreated.It can cause shock, coma, respiratory or heart failure, and even death.
Seek emergency care if you experience some or all of the symptoms of an allergic reaction after taking a dose of penicillin:
In rare cases, penicillin can cause acute interstitial nephritis, an inflammatory kidney disease most often caused by an abnormal immune response to the drug.Symptoms include nausea, rash, fever, lethargy, decreased urine output, fluid retention, and vomiting.Most cases are mild, but some can become severe and lead to acute kidney injury.
Like all antibiotics, penicillin is associated with an increased risk of C. difficile diarrhea.This is caused by the bacteria normally present in the gut being destroyed by antibiotics, thereby allowing the C. difficile bacteria to multiply.Most cases are mild and easily treatable, but C. difficile is known to cause severe fulminant colitis, toxic megacolon, and death in rare cases.
Penicillin is generally considered safe during pregnancy and breastfeeding.Evidence in humans is lacking, but animal studies suggest no risk of fetal harm.
If you are pregnant, planning to become pregnant, or breastfeeding, talk with your healthcare provider to fully understand the benefits and risks of using penicillin.
Many drugs can also interact with penicillin, usually by competing for renal clearance.This increases penicillin concentrations in the blood and the risk of side effects and drug toxicity.Other drugs can speed up the removal of penicillin from the body and reduce the drug’s effectiveness.
To avoid interactions, always let your healthcare provider know about any medicines you are taking, whether prescription, over-the-counter, nutritional, herbal, or recreational.
Subscribe to our daily health tips newsletter and receive daily tips to help you live your healthiest life.
Lobanovska M, Pilla G. Penicillin discovery and antibiotic resistance: lessons for the future?Yale Journal of Biomedical Sciences.2017;90(1):135-45.
Founou LL, Founou RC, Essack SY.Antibiotic resistance in the food chain: a developing country perspective.pre-microbes.2016;7:1881.doi:10.3389/fmicb.2016.01881
Post time: Mar-25-2022